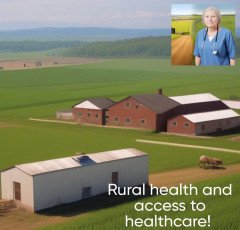
Rural Health And Access To Healthcare

In rural areas, which are often less inhabited and denserly populated than urban areas, the health status and healthcare delivery are referred to as rural health.
Geographic isolation, a lack of resources and healthcare professionals, as well as other issues, can make it difficult for rural residents to access healthcare.
Due to the scarcity of healthcare facilities and doctors, access to healthcare in rural areas can be extremely difficult.
Patients frequently have to travel great distances to obtain care in rural areas since there aren't enough healthcare facilities there. Those who have little mobility or money may find this to be very challenging.
Further, doctors, nurses, and other healthcare professionals are frequently in limited supply in rural locations. Finding a provider who can match their needs might be challenging for people as a result, particularly for specialized care.
Millions of people around the world are affected by major concerns related to rural health and access to healthcare.
Innovative approaches, such as the use of technology, telemedicine, and policy initiatives to increase access to treatment and support rural health, are needed to address these difficulties.
Rural populations could experience particular health issues and disparities in addition to the difficulties associated with the healthcare infrastructure and provider shortage. Obesity, diabetes, and other chronic diseases are frequently more prevalent in rural settings. Additionally, they could only have limited access to nutritious foods, opportunities for safe exercise, and other services.
Another significant area of concern in rural communities is mental health.
Additional pressures that rural inhabitants may experience include social isolation, a lack of access to mental health care, and a lack of privacy. These elements may contribute to greater prevalence of mental health problems, such as depression and suicide, in rural settings.
Rural health initiatives and programs have been formed globally to address these issues.
These initiatives seek to provide access to healthcare, attract and keep medical professionals in rural areas, and address the particular health issues that rural communities face. Additionally, by allowing patients in rural locations to get remote medical consultations and other healthcare services, telemedicine and other technology-based solutions can help close the access to care gap.
For everyone to have access to high-quality healthcare services and achieve the best possible health outcomes, regardless of where they live, it is imperative to improve rural health and access to healthcare.
Additionally important to enhancing rural health and access to healthcare are policy actions.
Through financial incentives, loan forgiveness programs, and other efforts, governments can help rural healthcare providers. Policies that encourage medical schools and residency programs to prioritize training and placement in these locations can also be put in place to boost the number of healthcare professionals working in rural areas.
Rural health issues and access to healthcare can also be successfully addressed by community-based strategies. For instance, peer-to-peer support groups and community health professionals can assist link rural residents to healthcare resources and offer support and education about their health.
Research is crucial for addressing the particular health issues that rural populations face and for creating workable solutions. More investigation is required to develop efficient therapies that might enhance health outcomes in these groups as well as to comprehend the underlying factors that contribute to health disparities in rural locations.
Rural health and healthcare access are serious problems that need complex solutions.
Effective rural health programs and efforts must address issues such as access to care, healthcare infrastructure, and provider shortages, as well as specific health issues and disparities that exist in rural areas. Healthcare professionals, decision-makers, academics, and community people can collaborate to better the health and wellbeing of rural populations all over the world.
The importance of socioeconomic determinants of health is another crucial part of rural health and access to healthcare. The economic and social factors that influence health outcomes, such as education, income, employment, housing, and transportation, are known as social determinants of health. Social determinants of health have the potential to significantly influence health outcomes and access to healthcare in rural locations.
Rural areas frequently have poor transportation, which can make it challenging for residents to receive medical treatment. The lack of work prospects in rural locations may also affect people's capacity to obtain health insurance and pay for medical services. Additionally, there might not be as many educational possibilities in rural locations, which might affect people's health literacy and their capacity to comprehend and use the healthcare system.
Improving rural health and access to healthcare requires addressing social determinants of health.
This can involve actions to expand accessibility to resources for education and health literacy, encourage economic growth and employment possibilities, and improve access to transportation. A more equitable healthcare system that caters to everyone's needs, no matter where they live, can be developed through addressing social determinants of health.
A thorough and multifaceted strategy that takes into account the particular difficulties faced by rural populations is needed to improve rural health and access to healthcare. This entails enhancing the healthcare system, addressing the shortage of healthcare professionals, putting policy initiatives into place, utilizing community-based strategies, doing research, and tackling social determinants of health. Together, we can build a healthcare system that is fair, easily accessible, and affordable.
The impact of technology in enhancing rural health and access to healthcare is another crucial factor to take into account.
The accessibility of healthcare in rural places could be significantly improved by developments in telehealth, remote monitoring, and digital health technologies. Telehealth enables virtual connections between patients and medical professionals in rural locations, saving travel time and enhancing access to specialized treatment.
Rural communities can benefit from digital health technologies, such as wearables and mobile health apps, to manage chronic illnesses, keep tabs on their health, and communicate with their healthcare professionals. These options can lower healthcare expenses while helping to improve health outcomes.
Recognizing that not all rural places have access to dependable internet and other digital infrastructure is crucial.
For technology-based solutions to be used effectively in these places, it is essential that all rural communities have access to high-speed internet and other digital resources.
A focus on community engagement and patient-centered care is necessary to improve rural health and access to healthcare in addition to technology-based solutions. Involving local communities in the development of healthcare programs and interventions can help to better understand their individual health needs and views.
Access to care and health outcomes can both be enhanced by patient-centered care, which emphasizes the value of including patients in their own healthcare decisions. This method can enhance patient happiness and involvement with healthcare services because it acknowledges the significance of patient preferences, values, and beliefs in healthcare decision-making.
The lack of healthcare infrastructure and providers, social determinants of health, access to technology, community involvement, and patient-centered care are just a few of the particular issues that must be addressed in order to improve rural health and access to healthcare. We can develop a healthcare system that accommodates everyone's requirements, irrespective of where they reside, by cooperating.
To take into account the linguistic and cultural diversity of rural residents and to make sure that healthcare is available and acceptable for their culture.
Indigenous and immigrant communities, which are prevalent in many rural locations, may encounter significant challenges in accessing healthcare services because of linguistic and cultural obstacles as well as a longstanding distrust of the healthcare system.
Healthcare systems and providers can provide linguistically and culturally relevant services, such as interpretation services and cultural competency training for healthcare professionals, to overcome these challenges. This can help to increase patient-provider communication and confidence while ensuring that healthcare services are customized to the specific requirements and viewpoints of different rural communities.
A comprehensive strategy that addresses the intricate and interwoven problems that rural communities confront is necessary to improve health and access to healthcare in rural areas. As part of this, healthcare infrastructure must be improved, provider shortages must be addressed, policy interventions must be put in place, community-based approaches must be used, research must be done, social determinants of health must be addressed, technology must be used to promote patient-centered care, and healthcare services must be available to all rural populations and be culturally appropriate. Working together, we can develop a more equitable and functional healthcare system that caters to everyone's needs, no matter where they may reside.
The design, implementation, and evaluation of healthcare initiatives in rural areas should incorporate and empower local populations in addition to the aforementioned strategies. Community people are involved in every step of the research process, from developing research questions to distributing findings, in community-based participatory research (CBPR).
By enabling local communities to actively participate in their own health and healthcare, CBPR can be a useful tool for involving people in improving rural health and access to healthcare. This method can assist in identifying the particular requirements and viewpoints of rural communities, which can result in the creation of healthcare solutions that are both more successful and culturally sensitive.
Must understand that enhancing rural health and healthcare access is a continuous process that demands persistent effort and dedication rather than a one-time event. To address the persisting issues encountered by rural people, more research, policy lobbying, and programming activities are required.
A comprehensive and long-term strategy is needed to address the difficult and varied task of improving rural health and access to healthcare.
As part of this, healthcare infrastructure must be improved, provider shortages must be addressed, social determinants of health must be addressed, technology must be used to its fullest potential, patient-centered care must be promoted, cultural and linguistic competence must be ensured, local communities must be involved through CBPR, and sustained investment and commitment must be made. We can develop a healthcare system that accommodates everyone's requirements, irrespective of where they reside, by cooperating.
The role of policy interventions is another factor to take into account in improving rural health and access to healthcare. Access to healthcare for rural communities can be significantly improved by policy changes at the federal, state, and municipal levels.
For instance, policies that encourage healthcare professionals to practice in rural areas can aid in addressing the scarcity of providers. These regulations may include loan forgiveness plans, tax breaks, and grants for healthcare professionals who opt to work in rural areas. Additionally, policies that encourage the hiring and education of healthcare professionals from remote areas may enhance access to linguistically and culturally competent care.
Expanding Medicaid eligibility and financing, investing in healthcare infrastructure, and addressing socioeconomic determinants of health like education, housing, and transportation are other policy actions that can enhance rural health and access to healthcare.
For low-income rural people that might not otherwise have access to affordable healthcare, expanding Medicaid eligibility and financing can assist enhance access to healthcare services. To make sure that healthcare services are accessible in rural areas, investments in healthcare infrastructure, such as rural hospitals and clinics, can be made.
A major factor in enhancing rural health and access to healthcare is addressing social determinants of health, such as housing, transportation, and education. For rural people that do not have access to dependable transportation, removing mobility obstacles can help to enhance access to healthcare services.
Access to healthcare and rural health can both be significantly improved by policy initiatives.
Policymakers can contribute to the development of a more equitable and efficient healthcare system that caters to the needs of rural populations by providing incentives for healthcare professionals to practice in rural areas, increasing Medicaid eligibility and funding, investing in healthcare infrastructure, and addressing social determinants of health.
The usage of technology is a crucial factor to take into account while trying to improve rural health and access to healthcare. Some of the obstacles to receiving healthcare in rural locations, such as transportation and distance, can be overcome with the aid of technology.
In rural locations where access to healthcare services may be limited, telehealth, or the use of technology to deliver remote healthcare services, can be very helpful. Among other modalities, telehealth can encompass videoconferencing, remote monitoring, and mobile health technologies.
By allowing patients to communicate with medical professionals from a distance, telehealth can expand access to healthcare services for rural communities.
This can lessen the need for patients to travel far to obtain care, which can be difficult for patients with restricted transportation.
By enabling healthcare professionals to give care remotely to patients in various locations, telehealth can assist to solve the shortage of clinicians in rural areas. This can lessen the pressure on individual clinicians and improve the effectiveness of healthcare delivery.
By giving healthcare professionals access to specialist knowledge and resources that may not be nearby, telehealth can help to raise the quality of healthcare services provided in remote locations. For instance, telemedicine enables medical professionals in rural areas to consult with experts at academic medical facilities or to gain access to clinical decision support technologies that can assist in guiding diagnoses and treatment choices.
In conclusion, technology can significantly contribute to the expansion of healthcare access and rural health. Health care providers and systems can increase access to healthcare services for rural populations, address provider shortages, enhance healthcare efficiency and quality, and get around some of the obstacles to accessing healthcare services in rural areas by utilizing telehealth and other technologies.







 Smart Doorbell
Smart Doorbell  NordPass
NordPass  Unlimited access to classes on illustration, photography, design, film, music
Unlimited access to classes on illustration, photography, design, film, music  ASPINAL LONDON
ASPINAL LONDON  RPM 3.0
RPM 3.0  One World Collection
One World Collection  Unreal Engine 5 For Beginners Learn The Basics Of Virtual Production
Unreal Engine 5 For Beginners Learn The Basics Of Virtual Production  SOFAS
SOFAS  SEO Checklist
SEO Checklist  Acer Laptop
Acer Laptop  Men Clothing
Men Clothing  The Secret Email System
The Secret Email System  Online Marketing
Online Marketing  NordVPN
NordVPN  Only For The United States
Only For The United States  Graphics & Design
Graphics & Design  The Click Engine
The Click Engine  Best Selling Books
Best Selling Books  Hot Bags For Pain Relief
Hot Bags For Pain Relief  Amazon Best Selling Products
Amazon Best Selling Products  Creative Brief For Video Shoot
Creative Brief For Video Shoot  NordLocker
NordLocker  TitTok Revolution
TitTok Revolution  All Wireless Products
All Wireless Products  BEST SELLER TOP10
BEST SELLER TOP10  Hello Theme
Hello Theme  Best Sellers On Amazon
Best Sellers On Amazon  Best Home Appliances
Best Home Appliances  Favorite Company (Cuelinks)
Favorite Company (Cuelinks)  ASUS Laptop
ASUS Laptop  Women Fashion
Women Fashion  1150+Trendy kids coloring pages Bundle
1150+Trendy kids coloring pages Bundle  Sennheiser
Sennheiser  ELECTRONIC ACCESSORIES
ELECTRONIC ACCESSORIES  Artificial Intelligence
Artificial Intelligence  Online Technology Classes
Online Technology Classes  Best Robotic Vacuum Cleaners
Best Robotic Vacuum Cleaners  Top Rated From Amazon
Top Rated From Amazon